HUG “Patients as Partners” relationship model
Sylvie Touveneau, leader of the Patients as Partners project
Context
A mutual recognition
What is the partnership model for the HUG?
Who is the patient partner?
Who are the other partners?
Conclusions
Context
With nearly 60,000 hospitalizations and 100,000 consultations in 2015, the partnership with the HUG is a shared concern.Collaboration with patients and caregivers in discussions, decisions, and actions related to their care becomes essential (FOPH Health Policy: Priorities of the Federal Council/Health Report 2020, January 23, 2013). The partnership is expressed through a change in the relationship, favoring a close collaboration between patients, their caregivers, and professionals. This approach has already been successfully adopted at the HUG in several sectors.As part of the 20/20 strategy, the “Patients as Partners” program is one of the key measures for improving quality of services. The goal is to promote this relationship model at each step of patient care, in all care specialties, as well as in areas such as hospitality, teaching, or governance.The brainchild of a team of multidisciplinary professionals and patients, the conceptual framework of the partnership is the first step of this project. It will be the tool for identifying areas and developing actions, for which patients and caregivers are recognized as stakeholders in the healthcare sector.It should be noted that the project team, which initially focused on care outcomes, subsequently integrated representatives from other areas of activity outside of healthcare.
A mutual recognition
Promotion of the HUG “Patients as Partners” model involves a paradigm shift. Today, the relationship mode is still too often paternalistic (The “Montreal model”: the challenges of a partnership relationship between patients and health professionals). Under the pressure of patients, increasingly well informed, and health professionals themselves, it moves towards a relationship based on trust, listening, dialog, mutual respect, and shared decision making. Everyone has their place and role in the same team.This development requires a repositioning of roles: the patient knows better than anyone what their symptoms are and how they experience these symptoms. Their view of the hospital and its services is that of a client. We can only treat the patient and make progress with them. The professional, for their part, no longer makes decisions alone, but instead seeks to collaborate with the patient.The partnership is consequently based on respect of the other, on a reciprocal recognition of skills and knowledge and of the experience of each partner. This synergy of the expertise of different stakeholders enables care and hospital stays to be improved.
A broad spectrum cooperation
In this collaborative context, patients are given legitimacy in their position as “stakeholders in health,” which most often (but not solely) materializes as “stakeholder in their own health.”In some cases, patients and their caregivers develop knowledge about the disease and decide to share this knowledge with other patients (through mentoring, speaking at a medical or association conference, etc.). In other cases, they are led to share their experience for the benefit of professionals (role play with medical students, colleague in a health care team, etc.) or even to join bodies to give their opinions. The spectrum of the partnership is indeed broad and opportunities to be a “stakeholder in the healthcare system” are growing quickly (participation in associations, lobbying in parliament, focus groups, inclusion in management committees, etc.).
What is the partnership model for the HUG?
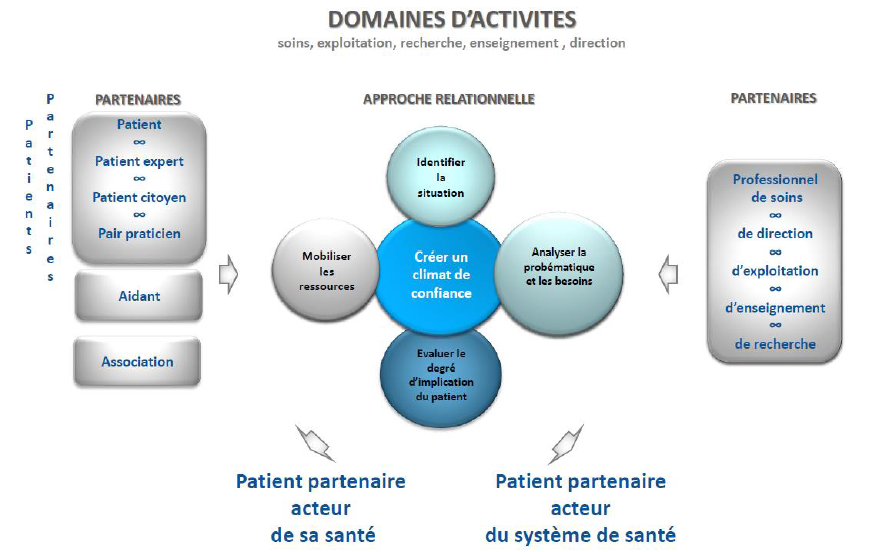
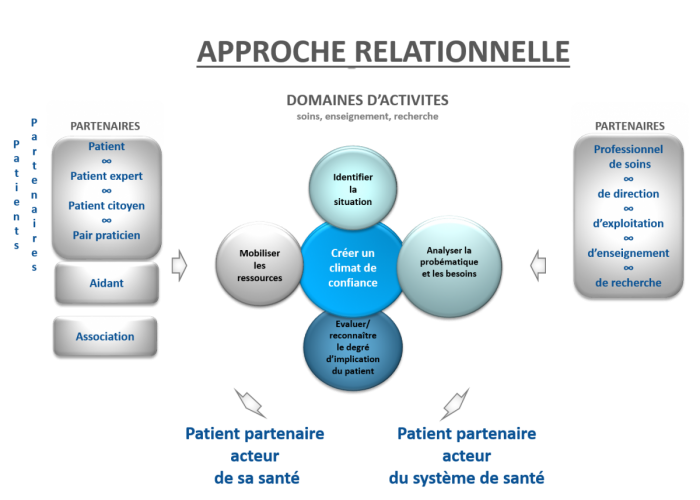
Since cooperation between patients and professionals can be embodied in different ways, the partnership approach encouraged at the HUG aims to be flexible.The diagram below illustrates this dynamic, multi-dimensional process:
Components of the partnership
The degree of involvement, personal capabilities, and the area of activity concerned are all elements that influence the nature of the partnership. However, the “recipe” can be adjusted depending on situations and given moments. The components of the collaboration are combined over the course of the relationship and do not necessary follow a specific order.
- Identifying the meeting situation: the patient, the caregiver, and the professional may have many opportunities to cooperate. Some examples: reception of a patient, the professionals who introduce themselves, announcing a diagnosis, a shared decision, the care agenda, participation in clinical research, improving the comfort of patients and caregivers.
- Evaluating the degree of involvement: based on the patient's needs and capabilities (Food for Thought, Portraits of Patients in 2024, FM), they can be involved in different ways. The type and degree of involvement varies, in particular based on their health status and their desire to enter into the relationship.How does the patient partner get involved?
- Analyzing the problems and the needs: the commitment of the partners, in an action that makes sense for each one, makes it possible to define the strategy. Consideration of individual factors such as age, culture, gender, behavior toward the disease, expectations in terms of communication, as well as other contextual economic factors and policies supplement this analysis.
- Mobilizing resources: whether at reception, during a consultation or a focus group, this involves mobilizing the skills, knowledge and aptitudes of patients and caregivers to express themselves, listen, decide, and/or act.Their ability to communicate, as well as their abilities to express their needs, fears and observations, must also be recognized.
- Creating a climate of trust: so that patients feel fully entitled to freely express themselves and to share aspects of their experience, professionals have the responsibility of creating a climate of trust conducive to the partnership. They are driven by values of empathy and mutual respect shared between partners. They use tools such as active listening and legitimization to practice participatory communication.
Who is the patient partner?
For health professionals, the patient partner is a patient, patient expert, patient citizen, and a peer practitioner. The same person can embody these different roles at different moments in their care pathway.
- The patient is a person whose physical and/or mental health requires the intervention of health professionals in order to recover their health.
- The patient expert shares their knowledge about the disease and treatments. This expertise acquired from experience with the disease and the hospital allows patients to develop an authentic partnership with professionals, to discuss or even question certain practices (Grimaldi, A. (2010). Les différents habits de l’ « expert profane » [The different roles of the “lay expert”]. Les tribunes de la santé, 2(27), 91-100). They are very well positioned to evaluate the quality of services and to identify potential improvements adapted to their needs. This shared experience may take place with other patient experts and in all areas of activities such as care, governance, hospitality, or communication.
- The patient citizen is involved in health policies, even in the development and revision of public health laws. The patient citizen demonstrates civic commitment and rallies around topics related to health.
- The peer practitioner is a person who has already experienced the disease and its treatment and who shares their experience with a “novice” patient, in order to support this patient. At this stage, the patient turned peer practitioner is able to take a step back and conceptualize from their experience. Peer practitioners receive certification training (Ecole d’études sociales et pédagogiques Lausanne [Lausanne School of Social and Pedagogical Studies], Haute école de travail social et de la santé Vaud [Vaud Higher School of Social Work and Health], Certificate of Peer Practitioners in Mental Health), on key aspects of a helping relationship (active listening, ethical principles of support, etc.) and supervision by qualified professionals.
The patient partner works with professionals to seek solutions adapted to problems concerning their health and their care plan or issues of health strategy. Certain conditions are necessary for this participation, such as patient-accessible quality information and an environment suitable for the expression of their experience, needs, and expectations.
Who are the other partners?
Beside the patient, other people may be involved in the partnership relationship at one time or another.
- The caregiver, family caregiver, support person, third party, or therapeutic representative and often friends and family members of patients. They may take the patient’s place - with the patient’s explicit agreement or in case of physical/psychological disability - and therefore be partners. They are emotional and social supports, but they also contribute to the patient’s care and to the improvement of the quality of the hospital. Guardians and trustees are included in this category.
- Associations: the role of patient associations is to break the isolation caused by the disease and to make known or recognize often little-known conditions. The patient association is gradually becoming a partner for physicians and healthcare institutions.
How does the patient partner get involved?
The nature and level of involvement varies depending on the moment or the patient’s situation. The patient can get involved at all levels of the institution, spontaneously or in response to an invitation, and intervene in care processes or societal issues.
- Presence: patients and their caregivers participate through their presence and their listening and meetings with professionals, at conferences, symposiums, etc.
- Expression/deliberation: patients and their caregivers express themselves in various ways (oral, written, art and social media). They are encouraged to participate in discussions related to patient care and to play an active role (Advancing Effective Communication, Cultural, Competence, and Patient).
- Decision making: patients and their caregivers share in decisions about them. They work together to identify the most reasonable care in a given context, while respecting their values and preferences.
- Action: patients and their caregivers act in a practical way. They are encouraged to get informed, to get involved, to express themselves, and to be active in the different areas of activity (Advancing Effective Communication, Cultural, Competence, and Patient).
Conclusions
Far from a narrow standardized approach, the proposed HUG Patients as Partners design is flexible, to embrace the diversity of situations. It focuses on the variability of relationship dynamics and possibilities for application. This openness and this design flexibility directly encourage professionals, from all fields of activity, to engage in this approach. They allow creative and “tailor-made” forms of collaboration.Promotion of the HUG Patients as Partners design is undoubtedly a way to enhance the participatory approaches undertaken by the professionals of the HUG. It also allows the transition from a traditional relationship approach toward a partnership approach to be assessed.
By committing to such an approach, professionals contribute to an open relationship and improved communication. Finally, the actions implemented create meaning and humanity for the patient.
Avec plus de de 60'000 hospitalisations et 100'000 consultations en 2015, le partenariat aux HUG est l’affaire de tous. La collaboration avec les patients et les aidants dans les discussions, décisions et actions liées à leurs soins devient essentielle (OFSP Politique de la santé : les priorités du conseil fédéral/Rapport santé 2020, le 23 janvier 2013). Le partenariat s’exprime par un changement de mode relationnel en faveur d’une collaboration accrue entre les patients, leurs aidants et les professionnels. Cette approche est déjà adoptée avec succès au sein des HUG dans plusieurs secteurs.
Dans le cadre de la stratégie 20/20, le projet « Patients partenaires » constitue une des pistes clé d’amélioration de la qualité des prestations. L’objectif est de promouvoir ce modèle relationnel à chaque étape de la prise en charge du patient, dans toutes les spécialités de soins, mais aussi dans les domaines tels que l’hôtellerie, l’enseignement ou la gouvernance.
Fruit de la réflexion d’une équipe de professionnels pluridisciplinaires et de patients, le cadre conceptuel du partenariat est la première étape de ce projet. Il sera l’outil d’identification des domaines et de développement des actions, pour lesquels les patients et les aidants sont reconnus dans leur position d’acteur de santé.
A noter que l’équipe de projet, au départ issue des soins, a intégré dans un deuxième temps des représentants d’autres domaines d’activités hors soins.
La promotion du modèle HUG « Patients partenaires » implique un changement de paradigme. En effet, aujourd’hui le mode relationnel reste encore trop souvent paternaliste (Le « Montreal model » : enjeux du partenariat relationnel entre patients et professionnels de la santé). Sous la pression des patients, toujours mieux informés, et des professionnels de la santé eux-mêmes, il tend vers une relation basée sur la mise en confiance, l’écoute, le dialogue, le respect mutuel et la décision partagée. Chacun y a sa place et joue dans la même équipe.
Cette évolution implique un repositionnement des rôles : le patient sait mieux que personne quels sont ses symptômes et comment il les vit. Son regard sur l’hôpital et ses prestations est celui du client. On ne peut le soigner et progresser qu’avec lui. Le professionnel, de son côté, ne décide plus tout seul, mais cherche davantage à collaborer avec le patient.
Le partenariat repose dès lors sur la considération de l’autre, sur une reconnaissance réciproque des compétences et du savoir et du vécu de chaque partenaire. C’est bien la complémentarité des expertises qui permet d’améliorer la prise en charge et les séjours à l’hôpital.
Une collaboration à large spectre
Dans ce contexte collaboratif, les patients sont légitimés dans leur position d’« acteur de santé » qui se décline le plus souvent en « acteur de sa santé », mais pas seulement.
Dans certains cas, les patients et leurs aidants s’approprient des connaissances sur la maladie et décident d’en faire profiter d’autres malades (parrainage, témoignage dans un congrès associatif ou médical, etc.). Dans d’autres, ils sont amenés à partager leur expérience au bénéfice de professionnels (jeux de rôle avec étudiants en médecine, collaborateur dans équipe soignante, etc.) ou même à intégrer des instances pour donner leurs avis. Le spectre du partenariat est en effet large et les occasions citoyennes d’être « acteur du système de santé » sont en plein essor (participation à des associations, lobbyisme au parlement, focus groupes, intégration dans des comités de gestion, etc.).
Parce que la collaboration entre patients et professionnels peut s’incarner de différentes manières, l’approche de partenariat préconisée aux HUG se veut souple et flexible.
Ce processus dynamique à dimensions multiples est illustré par le schéma ci-dessous :
Les ingrédients du partenariat
Le degré d’implication, ses capacités personnelles et le domaine d’activité concerné sont autant d’éléments qui influencent la nature du partenariat. Cependant, la « recette » reste modulable selon les situations et les moments. Les éléments constitutifs de la collaboration se combinent entre eux au fil de la relation et ne respectent pas nécessairement un ordre.
- Identifier la situation de rencontre : le patient, l’aidant et le professionnel peuvent être à l’initiative de nombreuses occasions de collaborer. Quelques exemples :l’accueil d’un patient, les professionnels qui se présentent, l’annonce d’un diagnostic, une décision partagée, l’agenda des soins, une participation à la recherche clinique, une amélioration du confort des patients et des aidants .
- Evaluer le degré d’implication : en fonction de ses besoins et de ses capacités (Matière à réflexion, portraits de patients en 2024, FM), le patient peut s’engager de différentes manières. Le type et le degré d’implication varient, notamment en fonction de son état de santé et de son souhait à entrer en relation.
Comment s'implique le patient partenaire ? - Analyser la problématique et les besoins : l’engagement des partenaires, dans une action qui fait du sens pour chacun, permet de définir la stratégie. La prise en compte des facteurs individuels tels que l’âge, la culture, le genre, le comportement face à la maladie, les attentes en matière de communication, mais aussi de facteurs contextuels économiques, politiques complètent cette analyse.
- Mobiliser les ressources : que ce soit à l’accueil, lors d’une consultation ou d’un focus group, il s’agit de mobiliser les compétences, le savoir et les aptitudes des patients et des aidants à s’exprimer, à écouter, à décider et/ou à agir.
Leur capacité à communiquer, comme celles de savoir exprimer ses besoins, ses craintes, ses observations doivent être également reconnues. - Créer un climat de confiance : afin que les patients se sentent pleinement autorisés à s’exprimer librement et à transmettre des éléments de leur vécu, les professionnels ont la responsabilité de créer un climat de confiance propice au partenariat. Ils sont portés par des valeurs d’empathie et de respect mutuel partagées entre les partenaires. Ils emploient des outils tels que l’écoute active et la légitimation pour pratiquer une communication participative.
Face aux professionnels de la santé, le patient partenaire se décline en patient, patient expert, patient citoyen et pair praticien. Une même personne peut incarner ces différents rôles à des moments différents de son parcours.
- Le patient est une personne dont la santé physique et/ou psychique nécessite l’intervention des professionnels de santé afin de retrouver sa santé.
- Le patient expert partage son savoir de la maladie et des traitements. Cette expertise acquise avec l’expérience de la maladie et le vécu hospitalier permet aux patients de développer un authentique partenariat avec les professionnels, de discuter, voire de mettre en question certaines pratiques (Grimaldi, A. (2010). Les différents habits de l’ « expert profane ». Les tribunes de la santé, 2(27), 91-100). Ils sont en effet très bien placés pour évaluer la qualité des prestations et identifier des pistes d’améliorations adaptées à leurs besoins. Ce partage d’expérience peut se faire avec d’autres patients experts et dans tous les domaines d’activités tels que les soins, la gouvernance, l’hôtellerie ou la communication.
- Le patient citoyen est impliqué dans les politiques de santé voire dans l’élaboration et la révision des lois de santé publique. Il fait preuve d’engagement citoyen et se mobilise autour de sujets en lien avec la santé.
- Le pair praticien est une personne qui a déjà expérimenté la maladie et ses traitements et qui partage son expérience avec un patient « novice », afin de le soutenir. A ce stade, le patient devenu pair praticien a su prendre du recul et conceptualiser à partir de son expérience. Des pairs praticiens bénéficient d’une formation certifiante (Ecole d’études sociales et pédagogiques Lausanne Haute école de travail social et de la santé Vaud Certificat de pairs praticiens en santé mentale), sur les éléments clés de la relation d’aide (écoute active, principes éthiques de l’accompagnement, etc..) et de supervisions par des professionnels qualifiés.
Le patient partenaire est celui qui construit avec les professionnels une recherche de solutions adaptées à des problématiques concernant sa santé et son projet de soins ou à des questions de stratégie de santé. Des conditions sont nécessaires à cette participation, telles qu’une information de qualité accessible au patient et un environnement propice à l’expression de son expérience, de ses besoins et de ses attentes.
A côté du patient lui-même, d’autres personnes peuvent être impliquées dans la relation de partenariat à un moment ou à un autre.
- L’aidant, le proche aidant, l’accompagnant, le tiers, le représentant thérapeutique sont souvent les proches des patients. Ils peuvent se substituer au patient - avec son accord explicite ou en cas d’incapacité physique/psychique - et donc être partenaires. Ils sont des soutiens émotionnels, sociaux, mais peuvent aussi contribuer à la prise en charge du patient et à l’amélioration de la qualité à l’hôpital. Le curateur et le tuteur sont intégrés dans cette catégorie.
- Les associations : le rôle des associations de patients est de rompre l’isolement provoqué par la maladie et de faire connaître ou reconnaître des affections souvent mal connues. L’association de patients est devenue progressivement un partenaire pour les médecins et les institutions de santé.
Comment s’implique le patient partenaire?
La nature et le niveau d’implication varient selon le moment ou la situation où se trouve le patient. Celui-ci peut s’engager à tous les niveaux de l’institution, spontanément ou en réponse à une invitation, et intervenir sur des processus de soins ou des sujets de société.
- La présence : les patients et leurs aidants participent par leur présence et leur écoute à des entretiens avec des professionnels, à des conférences, à des colloques, etc.
- L’expression/délibération : les patients et leurs aidants s’expriment de diverses manières (oral, écrit, art et médias sociaux). Ils sont encouragés à participer aux discussions liées à la prise en charge du patient et à y prendre une part active (Advancing Effective Communication,Cultural, Competence,and Patient).
- La décision : les patients et leurs aidants partagent les décisions les concernant. Ils collaborent ensemble afin d’identifier la prise en charge la plus raisonnable dans un contexte donné, et dans le respect de leurs valeurs et préférences.
- L’action : les patients et leurs aidants agissent de manière concrète. On les encourage à s’informer, à s’engager, à s’exprimer et à être actifs dans les différents domaines d’activités (Advancing Effective Communication,Cultural, Competence,and Patient).
Loin d’une démarche standardisée étroite, le concept HUG Patients partenaires proposé se veut souple pour embrasser la diversité des situations. Il mise sur la variabilité de la dynamique relationnelle et des possibilités d’application. Cette ouverture et cette flexibilité conceptuelles sont à même d’encourager les professionnels, de tous domaines d’activités, à s’engager dans cette approche. Elles autorisent des formes de collaboration créatives et « sur mesure ».
La promotion du concept HUG Patients partenaires constitue sans aucun doute un moyen de valoriser les démarches participatives entreprises par les professionnels des HUG. Elle permet également d’évaluer la transition d’une approche relationnelle traditionnelle vers une approche de partenariat.
En s’engageant dans une telle démarche, les professionnels contribuent à l’ouverture relationnelle et à l’amélioration de la communication. Au final, les actions mises en place gagnent en sens et humanité pour le patient.

